Understanding Pressure Ulcers: Causes, Stages, and Modern Treatment Options

Pressure ulcers are more than just a medical buzzword; they have a real and lasting impact on quality of life—for patients, caregivers, and healthcare systems alike.
Whether you’ve heard them called bedsores, pressure injuries, or decubitus ulcers, these preventable wounds are a familiar challenge, especially in aged care, hospital settings, and for anyone with limited mobility.
In Australia, proactive prevention and modern treatment are at the heart of best practice care. Let’s break down what pressure ulcers are, why they happen, what the four stages look like, and the practical, science-backed ways to prevent and manage them—including some of the modern wound care innovations making a genuine difference.
What Are Pressure Ulcers and Why Do They Matter?
Pressure ulcers, also commonly referred to as pressure sores or bedsores, are areas of skin and underlying tissue damage caused by sustained pressure or a combination of pressure with friction and shear.
Most often, these injuries develop where the skin covers bony prominences—think the tailbone, heels, hips, and elbows—due to long hours lying in a bed or sitting in a chair without enough movement.
Anyone can develop a pressure ulcer, but certain groups are much more at risk—people with impaired mobility, such as the elderly, individuals living with chronic diseases (like diabetes or heart failure), and people recovering from surgery or injury who spend extended periods in bed.
In healthcare settings, pressure ulcers are not just a quality of life issue; they’re also a marker of care standards, affecting physical comfort, emotional well-being, long-term recovery, and, in worst cases, survival.
What Causes Pressure Ulcers? The Underlying Science
At their core, pressure ulcers occur when prolonged pressure over an area of skin squeezes tiny blood vessels shut. Without adequate blood flow—and therefore, oxygen and nutrients—cells begin to die, tissues break down, and wounds form.
But pressure itself isn’t the only player. The full picture includes:
- Pressure: Direct, unrelieved force against a surface (like a mattress) that restricts blood flow. Even relatively mild, constant pressure (as little as 32 mmHg) can start to cause damage in just 1-2 hours.
- Friction: Skin rubbing against a surface—such as bedsheets or wheelchair cushions—can damage the outer layer, especially when the skin is damp.
- Shear: When deeper tissue moves in one direction, while the skin stays put—often while sliding down a raised bed—deeper blood vessels are stretched and pinched off, increasing the risk of tissue death.
- Moisture: Sweat, urine, feces, or wound drainage can soften skin and raise the risk of breakdown. Incontinence is a major risk factor.
In the body, these forces trigger a chain reaction known as ischaemia (lack of blood supply), cellular death, and inflammation. If pressure is not relieved, the cycle continues, progressing from skin redness to open sores, and in serious cases, deep wounds exposing muscle or bone.
Who Is at Risk for Pressure Ulcers? Key Factors to Know
The risk of developing pressure ulcers goes up significantly in those who:
- Can’t move easily on their own (due to illness, paralysis, sedation, surgery, or frailty)
- Have decreased or altered feeling, so they may not sense pain and shift position (as in spinal cord injuries, neuropathy, or advanced diabetes)
- Suffer from poor nutrition or dehydration, which weakens skin and slows healing
- Manage chronic illnesses that interfere with circulation (e.g., vascular disease, heart or kidney failure).
- Experience incontinence, leading to constant skin dampness
- Are over 70 years old—skin thins and takes longer to heal with age
Risk assessment tools like the Braden Scale or Norton Scale are used in hospitals and aged care to systematically identify those most vulnerable, examining factors like sensory perception, moisture, activity, mobility, nutrition, and friction/shear. Early action for at-risk individuals is essential to stop pressure injuries before they start.
The Four Stages of Pressure Ulcers: What to Look For
Pressure ulcers are classified by their severity, guiding both diagnosis and treatment. Let’s walk through the distinctive features of each stage:
Stage 1: Warning Redness—The Earliest Sign
- What it looks like: Intact, unbroken skin with a persistent area of non-blanchable redness (doesn’t turn white when pressed) over a bony prominence. In darker skin tones, the area may appear blue or purple rather than red.
- How it feels: The site may feel warmer or cooler than nearby skin, or firmer/softer. People often report pain, tingling, or itching.
- Key difference: Unlike normal redness from brief pressure, this redness doesn’t fade promptly and signals underlying tissue damage.
- Why it matters: Stage 1 is fully reversible and, with prompt action, usually heals within 1–2 days. This is the critical intervention point.
Stage 2: Open Wounds and Blisters—Partial Skin Loss
- What it looks like: The skin breaks open, revealing a shallow, open wound with a red or pink base, or an intact/ruptured blister filled with clear fluid. Only the epidermis (outer layer) and part of the dermis (second layer) are involved.
- Distinguishing features: There may be some swelling, pus, or drainage, but fat, muscle, or bone aren’t visible.
- Symptoms: The area is painful, may be swollen, warm, and tender to touch.
- Progression: If not treated effectively, stage 2 ulcers can worsen rapidly, so early wound care is vital.
Stage 3: Deep Craters—Full-Thickness Loss
- What it looks like: The wound extends through all layers of the skin into the fat (subcutaneous) layer, forming a deep crater. Muscle, tendon, and bone are not visible yet.
- Additional signs: The wound may feature rolled edges, visible yellowish tissue (slough), and sometimes pus, a foul odour, or signs of infection.
- Risks: There may be tunnelling or undermining beneath the skin. The risk of complications such as bone infection or sepsis increases significantly at this stage.
- Time to heal: Weeks to months with consistent, advanced wound care.
Stage 4: The Most Severe—Muscle and Bone Exposed
- What it looks like: The wound is deep enough to expose muscle, tendon, ligament, or even bone. These ulcers may have extensive dead tissue (eschar), slough, and visible undermining/tunnelling of tissue under the wound’s edges.
- Symptoms: Often extremely painful or, paradoxically, numb if nerve damage has occurred.
- Complications: High risk of critical infections. Stage 4 ulcers may require surgical intervention, amputation, or long-term hospitalisation. Healing can take months to years and may not be complete.
Other Special Categories:
- Unstageable: If the wound bed is covered by dead tissue (eschar or slough) so the true depth can’t be determined.
- Suspected Deep Tissue Injury: A blood-filled blister or area of persistent, dark discolouration, often turning into a deeper wound rapidly beneath intact skin.
Table: Stages of Pressure Ulcers at a Glance
| Stage | Skin Condition | Features | Tissues Involved | Healing Time* |
|---|---|---|---|---|
| 1 | Intact, non-blanchable red | Pain, warmth, or firmness, no open wound | Upper skin | Days to week |
| 2 | Partial thickness loss | Open wound or blister, pink/red base | Epidermis & dermis | 1–3 weeks |
| 3 | Full thickness loss | Deep crater, fat tissue visible, possible slough | Through skin into fat | Weeks to months |
| 4 | Full thickness & beyond | Exposed muscle/bone/tendon, extensive tissue loss | Muscle, bone, ligament | Months to years |
*Approximate and dependent on overall health, care quality, and presence of complications.
Understanding the staging is crucial because the right treatment and prevention strategies can halt early ulcers in their tracks, but advanced sores demand complex wound management and increase a person’s vulnerability to major, sometimes fatal, infection.
Pressure Ulcer Prevention: What Really Works?
The number one “treatment” for pressure ulcers is prevention. Australian clinical and international guidelines strongly advocate a proactive, risk-based approach. Here’s what works in the real world:
1. Regular Repositioning
Turning and shifting position is the front-line defence. People confined to bed should be repositioned at least every two hours (shorter intervals for those at higher risk), and those in chairs should shift weight every 15 minutes. Use supportive devices such as pillows, foam wedges, or heel protectors to fully offload bony prominences.
2. Skin Care and Hygiene
Healthy skin is less likely to break down. Keeping skin clean and dry, using pH-neutral, fragrance-free cleansers, and gently patting dry is essential. Avoid vigorous rubbing, which can damage fragile skin. Apply moisturisers regularly, especially to dry areas, and clean the skin after every episode of incontinence.
3. Incontinence Management
Moisture and exposure to bodily fluids rapidly increase pressure sore risk. Use highly absorbent incontinence products, implement regular toileting schedules, and apply barrier products like creams and films to protect the skin. Products such as pressure ulcer creams and skin barriers like Cavilon No Sting Barrier Film help reduce irritation, especially in high-risk individuals.
4. Nutrition and Hydration
Ensuring adequate hydration and a balanced diet rich in protein, vitamins A and C, and zinc supports skin integrity and speeds healing. Malnutrition can both predispose to and delay the healing of pressure injuries—dietitian involvement is often essential.
5. Pressure-Redistributing Surfaces
Investing in modern support surfaces is one of the best ways to lower the risk of new pressure ulcers and promote healing of existing ones.
Pressure Mattresses and Pressure Ulcer Beds
- What are they? Specially designed mattresses (sometimes for entire beds) that distribute or alternate body pressure, reducing sustained force on any one area.
- Why are they important? Standard mattresses can intensify risk—even turning every two hours may not be enough for high-risk patients. Pressure mattresses and pressure ulcer beds are essential for at-risk persons, especially those with limited independence or advanced mobility challenges.
Types explained:
- Reactive (static) surfaces: Made of high-specification foam, gel, or air; respond to body weight and movement but do not actively change pressure points unless the person moves.
- Active (alternating) surfaces: Motor-driven air mattresses that actively change pressure points by inflating/deflating internal bladders on a set cycle.
Australian best practice:
The latest clinical guidelines (2025) and hospital protocols recommend considering a high-specification mattress or overlay for all at-risk individuals, and for anyone with an existing pressure ulcer; the surface chosen should be tailored to individual needs and comfort.
Practical Considerations:
- Don’t use doughnut cushions—they can actually increase damaging pressure at the edges!
- Combine specialty surfaces with regular movement for best results.
- Comfort and user acceptability matter—if a surface is uncomfortable, it will be used less consistently. Patient involvement in selection improves adherence and outcomes.
Modern Treatment Options for Pressure Ulcers
Treatment must be tailored to the stage and unique features of each ulcer, focusing on relieving pressure, maintaining a clean wound environment, managing pain, and supporting the body’s ability to heal—ideally, under the guidance of a wound care specialist.
Pressure Dressings and Wound Care Products
A cornerstone of pressure ulcer care is selecting the right wound dressing for each stage and wound type. Modern options include:
Foam Dressings
- What are they? Soft, absorbent material to cushion and protect wounds with moderate to heavy exudate, such as Allevyn Gentle Dressings.
- Use: Stage 2–4 ulcers with exudate (wound ooze). Foam dressings provide a moist, healing environment and can remain in place for several days, reducing discomfort and minimising dressing changes. Their gentle silicone adhesive is skin-friendly and allows pain-free removal for fragile skin.
Transparent Film Dressings
- E.g., Tegaderm: These are thin, see-through films that stick to the skin around the wound but not to the wound bed itself.
- Use: Ideal for superficial injuries, minor stage 1–2 pressure ulcers, or as a secondary dressing over foam or hydrogel dressings. They create a barrier against bacteria and moisture, allow direct wound observation, and are easy to remove.
- Considerations: Not for heavily exuding wounds. Excessive fluid can cause dressings to lift or trap moisture.
Hydrocolloid/Hydrogel Dressings
These are occlusive dressings that maintain moisture, support autolytic debridement (removing dead tissue), and are suitable for stage 2 or shallow stage 3 wounds with low to moderate exudate.
Barrier Films
Cavilon No Sting Barrier Film: Forms a breathable, transparent protective layer on skin, especially valuable for preventing and treating moisture damage (incontinence-associated dermatitis). Non-stinging, hypoallergenic, and suitable for use around wounds, stomas, and under dressings.
Pressure Ulcer Creams/Ointments
Purpose: Protect and repair the skin, especially early-stage ulcers or periwound skin (around the wound). Zinc oxide-based creams, silicone-based protectants, and specialised pressure ulcer creams create a barrier to moisture and help soothe irritated skin. There’s growing evidence for their use to prevent further skin breakdown but less evidence for accelerated healing in advanced stages.
Alginate and Hydrofibre Dressings
For wounds with high exudate (Stage 3–4). These dressings can absorb large amounts of fluid and help keep the wound bed moist without causing maceration to the surrounding skin.
Silver-Containing or Antimicrobial Dressings
Used if there’s infection or high risk of infection. Silver dressings, honey-impregnated dressings, and iodine-based options can help control bacteria.
Featured Products: Making Sense of the Options
Here’s a closer look at some leading choices in evidence-based pressure ulcer care:
1. Allevyn Gentle Foam Dressing

Allevyn Gentle is a triple-layered, silicone-based foam dressing designed for fragile or sensitive skin. It:
- Gently absorbs wound exudate, keeping damage at bay while providing a moist healing environment.
- Reduces pain and trauma during dressing changes, owing to a gentle silicone adhesive.
- Can be left in place for up to seven days depending on wound condition and exudate level, thus requiring fewer dressing changes and promoting patient comfort.
Clinical uses: Ideal for moderate to heavily exuding pressure ulcers and wounds at risk of further trauma.
2. Tegaderm Transparent Dressing
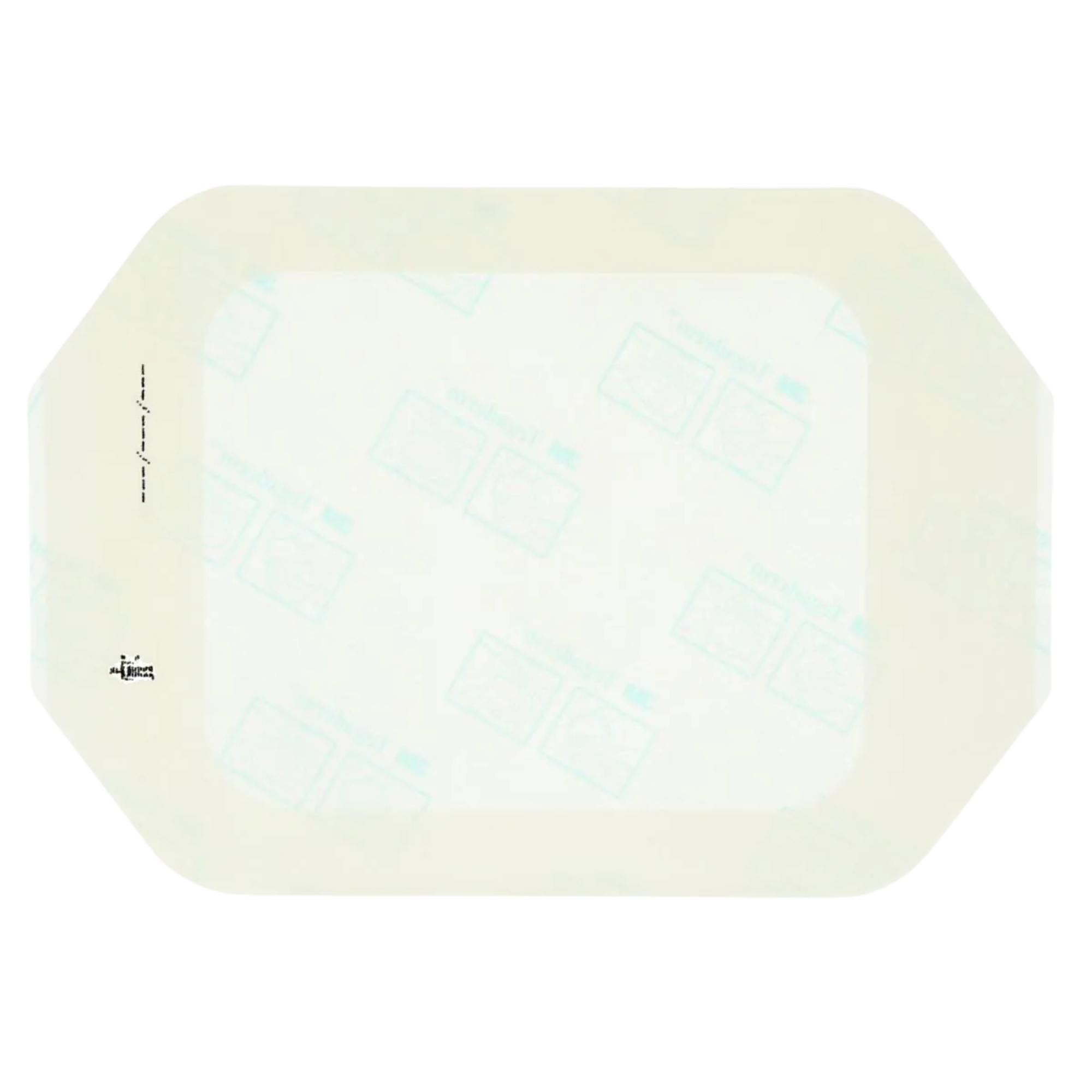
The Tegaderm transparent film dressing is lightweight, waterproof, and allows ongoing wound inspection without removing the dressing. It is:
- Suitable for superficial Stage 1–2 sores, donor sites, and as a secondary cover over other dressings.
- Helpful for securing IV or catheter sites in patients at risk of device-related pressure injuries.
- Long-wearing with low trauma on removal, making it ideal for patients with sensitive skin.
3. Cavilon No Sting Barrier Film

Cavilon is a spray or wipe-on film that creates a breathable, waterproof barrier protecting skin from irritation caused by moisture, friction, or adhesive dressings. It is:
- Suitable for both intact and damaged skin
- Alcohol-free and non-stinging, making it appropriate for repeated use
- Useful for periwound areas of pressure ulcers to shield from leakage, dressing adhesives, and bodily fluids.
Table: Modern Pressure Ulcer Management Products
| Product Name | Key Function | Best For |
|---|---|---|
| Pressure ulcer bed | Pressure redistribution during rest | Prevention for bed-bound people |
| Pressure mattress | Alternating/reducing pressure points | At-risk or ulcer management |
| Pressure ulcer cream | Skin protection and moisturising barrier | Early-stage or periwound care |
| Pressure dressing | Maintaining a moist environment, exudate control | All stages depending on type |
| Allevyn dressing | Moisture control, gentle adhesion, exudate absorption | Moderate-to-heavy exuding ulcers |
| Tegaderm | Transparent, waterproof, observation | Stage 1–2 and secondary dressing |
| Cavilon | Barrier film, moisture protection | Preventing irritation, periwound care |
Each of these products aligns to a specific stage or facet of pressure ulcer prevention and management. Matching product type and care techniques to an individual’s needs yields the best outcomes and comfort.
Australian Guidelines and Best Practice
Australian clinical pathways for addressing pressure ulcers emphasise:
- Screening all patients for risk early, with regular reassessment, especially following illness, surgery, or changes in mobility
- Developing prevention and wound management plans tailored to the individual—in collaboration with families and multidisciplinary teams (nurses, doctors, dietitians, physiotherapists)
- Focusing on early use of pressure-redistributing beds, high-grade mattresses, support cushions, and proper positioning techniques
- Keeping skin clean, dry, and well-moisturised while using evidence-based dressings for moist wound healing
- Providing consistent, well-documented care and education for both healthcare staff and carers
As of 2025, Australian clinical guidelines are regularly updated, supporting use of the latest international standards led by groups like the Pan Pacific Pressure Injury Alliance (PPPIA), the National Pressure Injury Advisory Panel (NPIAP), and the European Pressure Ulcer Advisory Panel (EPUAP).
Practical Tips: Small Changes, Big Impact
- Check your skin every day, especially if you’re at risk—look for red spots, colour or texture changes, pain, or warmth over bony points.
- Get moving as much as possible, even small shifts in position help! If you need assistance, ask carers for help with a schedule.
- Layer up protection: Use absorbent pads for moisture, pressure dressings for wounds, and cushions or mattresses designed for pressure relief. Avoid sitting on hard or wrinkled surfaces.
- Speak to your healthcare provider about diet and hydration needs to build a strong foundation for healthy skin.
When to Get Professional Help for Pressure Ulcers
Always contact your healthcare provider if you:
- Notice any skin changes that don’t improve within a day or two
- See open sores, worsening swallowing, fever, or foul-smelling drainage
- Experience pain or discomfort that’s new or unexpected
- Are caring for someone at home who develops any of the above signs
Prompt intervention can halt or reverse injury progression, dramatically reducing the risk of complications. For advanced ulcers (Stage 3–4) or wounds not healing as expected, referral to a specialist wound care nurse or wound clinic is crucial.
Taking Action Against Pressure Ulcers
Pressure ulcers are largely preventable complications with significant impacts on people’s lives, healthcare resources, and community well-being. Early recognition of risk, committed preventative care—including regular movement, skin protection and specialist support surfaces—as well as use of modern dressings and topical products, can make all the difference.
If you or a loved one is at risk, champion a proactive approach. Ask about pressure ulcer beds, pressure mattresses, and wound care solutions that fit personal needs. Remember, these wounds are not just a sign of ageing or illness—they’re a call for evidence-based, compassionate care and, above all, prevention.
Disclaimer: Platinum Health is not a hospital, clinic, or medical research organisation. We are a healthcare supplies store, and we only use publicly-available information from reliable medical references in this article. For tailored medical care, please consult your healthcare provider.
